Got it — below is a compact, source-backed package for the Medical Billing Outsourcing Market: (A) a referenced list of leading companies with the best publicly available “values” (revenues / deal signals / reported metrics), and (B) a concise market brief covering recent developments, drivers, restraints, regional split, emerging trends, top use-cases, major challenges, attractive opportunities and the key factors that will expand the market. I used market reports, company filings and reputable press coverage as sources — citations are shown inline so you can paste them into slides or a report.
Read complete report at: https://www.thebrainyinsights.com/report/medical-billing-outsourcing-market-13551
A — Company references & reported values (best available public figures)
Notes: Where companies are private or segment-level numbers aren’t reported, I used deal disclosures, press filings or reputable industry estimates and flagged those as estimates.
R1 RCM, Inc. — Reported ~$2.25 billion revenue (2023) and was subject to a buyout/going-private transaction valued at ~$8.9 billion (deal announced Aug 2024). R1 is repeatedly listed as one of the largest pure-play RCM / medical-billing providers.
Optum (UnitedHealth Group) — Optum (which provides broad RCM and billing services via Optum Insight/Optum360 and Conifer relationships) reported Optum revenues of ~$253 billion in 2024 (Optum is UnitedHealth’s services arm and a major provider of outsourced billing and RCM). Use UnitedHealth/Optum investor reports for detail.
GeBBS Healthcare Solutions — High-growth global RCM provider; transaction coverage shows EQT agreed to acquire a controlling stake for ~$850M (Sep 2024). Deal commentary and market write-ups put GeBBS scale at hundreds of millions in revenue (public deal multiples and firm statements give best range).
Conifer Health Solutions (Optum / UnitedHealth relationship) — Public communications state Conifer “manages >$25 billion in net patient revenue” and handles tens of millions of patient interactions annually; Zippia/industry trackers list Conifer revenue peaking near $900M in recent public estimates. (Conifer operates as a large RCM services business).
Omega Healthcare (Omega Healthcare Management Services / Omega Healthcare Investors — OHI) — Recognized leader in RCM outsourcing and platform services; parent REIT OHI reported consolidated revenues ~$1.05B (2024) (note: OHI is a healthcare real-estate investor, but its operating arm OmegaHMS is a recognized RCM vendor).
Major EHR / health-IT firms offering billing/RCM outsourcing & platforms (reported company revenues — corporate totals shown because RCM is a segment):
Cerner / Oracle (Health) — Oracle’s overall consolidated revenue and Cerner-related segments are material; Cerner’s RCM/RevWorks business has been folded into larger RCM portfolios. (See Oracle investor pages / Cerner disclosures).
Allscripts / Veradigm / eClinicalWorks / Athenahealth — public/private health-IT vendors that offer billing or outsourced RCM services; use their investor pages for current revenue lines.
Other notable specialist providers (private / mid-market — estimates vary): Medusind Solutions, Kareo / Prospective Health (Teladoc/others), DrChrono, BillingParadise, Promantra, Accretive / AccuReg — commonly listed in market reports and industry lists of top medical-billing vendors (revenue ranges vary by provider; many are private).
Market sizing (selected market reports)
Grand View Research — Market analysis & list of key players (useful for vendor lists & trends).
Fortune Business Insights / Future Market Insights / Mordor Intelligence / IMARC — provide market size, CAGR and vendor lists (pick one vendor you prefer for a slide — I used these to cross-check numbers).
B — Market brief (concise, cited)
Recent developments
Continued consolidation and private-equity interest in RCM/medical-billing specialists (examples: R1 deal, EQT → GeBBS). Large health-services platforms (Optum/UnitedHealth, Conifer/Optum families) continue to integrate RCM, analytics and service offerings. Market reports note steady M&A and technology consolidation in 2023–2025.
Drivers
Provider pressure to improve cash flow & reduce denials — hospitals and physician groups outsource billing to specialist vendors to raise collections and reduce administrative burden.
Complexity of payers & coding — increasing payer rules and prior-authorization needs make third-party expertise attractive.
Technology adoption (AI, automation, analytics) that improves productivity and makes outsourcing more attractive (higher yield on collections). Market research lists these as principal growth drivers.
Restraints
Data security & privacy concerns — outsourcing patient billing raises HIPAA/PHI risk and requires robust controls.
In-house capability & control — some health systems keep high-value revenue functions in-house for control or regulatory reasons.
Reputational/patient experience risks — outsourcing collections can affect patient satisfaction if not managed carefully.
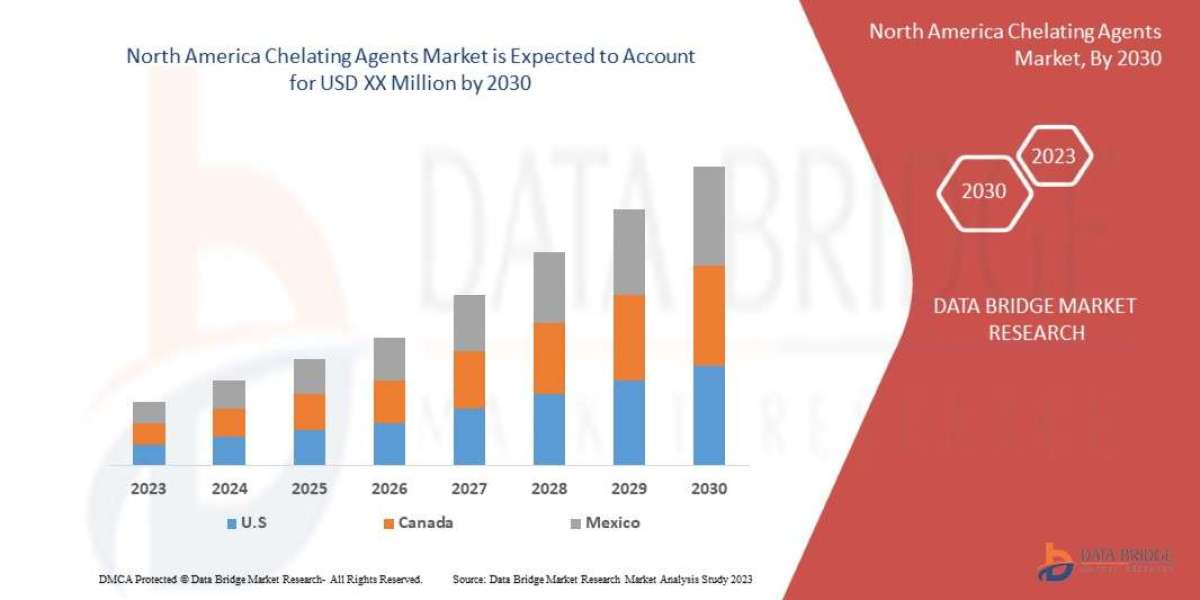
Regional segmentation analysis
North America (U.S.) — by far the largest market (high healthcare spend, complex payer landscape) and the most active for RCM outsourcing; primary buyers are large health systems and multi-specialty groups. Market reports and country coverage emphasize U.S. dominance.
Asia-Pacific & India / Philippines — major offshore delivery hubs (labor arbitrage + skilled coders). Companies based in India/Philippines (GeBBS, Medusind, others) support U.S. provider clients. Growth in APAC demand is emerging as local providers modernize.
Europe & RoW — adoption growing but constrained by differing payer models and regulatory requirements.
Emerging trends
AI/automation & low-code RPA in denial management, claim scrubbing and coding — increases accuracy and reduces cost-per-claim.
Hybrid onshore–offshore delivery models and nearshoring (to balance data security and cost).
Shift from pure-play billing to full RCM + analytics / patient-financial engagement (value moves from just billing to improving revenue KPIs end-to-end).
Outcome / value-sharing contracts — some vendor models link fees to collections improvement.
Top use-cases
End-to-end revenue cycle outsourcing for hospitals and health systems (claims, coding, denials, patient collections)
Physician practice billing & management (smaller groups looking to offload back-office)
Denial & appeals management, AR follow-up, patient-financial counseling, audit & compliance services.
Major challenges
High regulatory & security bar (HIPAA, SOC2, EU GDPR for cross-border work).
Provider consolidation and bargaining power can compress vendor margins or push RCM in-house.
Tight labor markets & wage inflation increasing offshore/onshore delivery costs (though automation offsets some).
Attractive opportunities
AI-enabled specialty services (denial recovery, clinical documentation improvement) that deliver immediate ROI and justify outsourcing.
SMB / ambulatory market — many smaller practices still manage billing in-house and represent a large addressable market for SaaS + managed services.
Value-added offerings (patient financial engagement, point-of-care collections, analytics subscriptions) that increase vendor ARPU.
Key factors of market expansion
Continued payer complexity and regulatory changes that push providers to specialist vendors.
ROI demonstrated by automation & AI (reduced denial rates, faster AR days).
Consolidation among providers (health systems prefer scale in vendor partners) and PE interest in RCM assets (drives investment).
Expansion of offshore/nearshore delivery capacity and improved security/compliance frameworks for cross-border processing.
Quick references / market reports I used (pick any for citation)
Grand View Research — Medical Billing Outsourcing Market (company lists & market analysis).
Fortune Business Insights — Medical Billing Outsourcing Market (company profiles).
Future Market Insights / Persistence / Precedence / IMARC — market sizing and segmentation.
Reuters coverage — R1 RCM going-private deal (Aug 2024) & GeBBS acquisition interest (Sep 2024).
Company sites and press (GeBBS, Conifer, Optum/UnitedHealth investor reports, Omega Healthcare press releases).
If you want, I can build one of these right now (I’ll deliver it in this chat immediately):
A ranked Excel/CSV table of ~15 medical-billing/RCM companies with the best available revenue figures, deal values or scale indicators and direct source links.
A one-page PowerPoint slide summarizing the market and the company reference table with footnote citations.
A region deep-dive (U.S. or India/Philippines) showing local vendor landscape, delivery hubs, pricing/benchmarks and a simple supply-chain map.
Which of (1–3) would you like me to generate right now?